COVID-19 & ARDS (Acute Respiratory Distress Syndrome)
Daily thoughts & numbers on the COVID-19 pandemic from a M.D. working in the front lines at the Emergency Department in a hospital in Stockholm, Sweden.
What we noticed at the hospitals is that it’s not just older people with underlying diseases that can get critically ill from COVID-19, there is another group of 30 to 70 year old (men) who smoke with hypertension that are also at risk of ending up at the ICU.
What we noticed is that even people in their twenties and thirties, men and women, can also get severe pneumonia with ARDS (although an even smaller sample than the one above – yet not an insignificant number however).
Even though the fatality rate is exceedingly low for people below 70 years of age with few underlying comorbidities, they still represent their fair share of patients treated at the ICU.
So far, of the 416 COVID-19 patients treated at the ICUs in Sweden we have the following numbers (unfortunately just age included in these numbers and not comorbidity/underlying diseases): *
- 20-29 yrs: 3,4% (15 patients)
- 30-39 yrs: 3,8% (16 patients)
- 40-49 yrs: 10,6% (44 patients)
- 50-59 yrs: 25,2% (105 patients)
- 60-69 yrs: 30,5% (124 patients)
- 70-79 yrs: 22,3% (93 patients)
- 80-89 yrs: 4,6% (19 patients)
Data above taken from SIR (Swedish Intensive Care Registry):
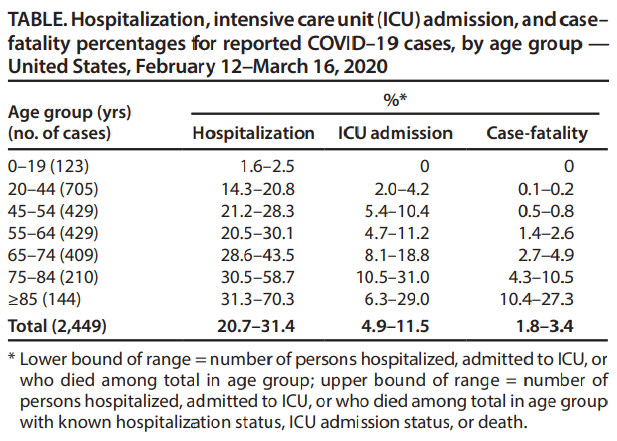
Similar numbers has been seen in other countries such as in USA: *
I can’t find any numbers/studies on ICU admission, age, AND comorbidity. But at my clinic and from the case-reports from other countries, many of the younger COVID-19 patients being admitted to the ICU don’t have any serious underlying diseases.
Sources:
- Severe Outcomes Among Patients with Coronavirus Disease 2019 (COVID-19) — United States, February 12–March 16, 2020
- SIR — (Swedish Intensive care Registry)
COVID-19 Numbers Sweden 2020-03-31 *
- 180 deaths nationally
- 103 of them in Stockholm
- 4 435 confirmed cases nationally

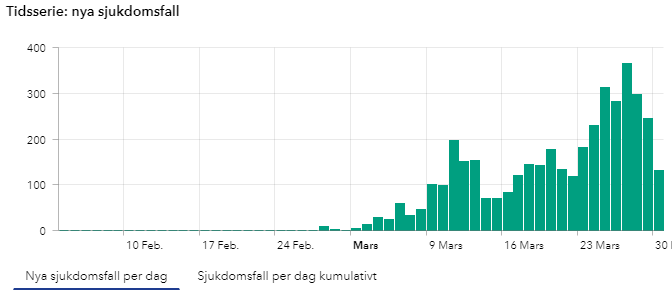
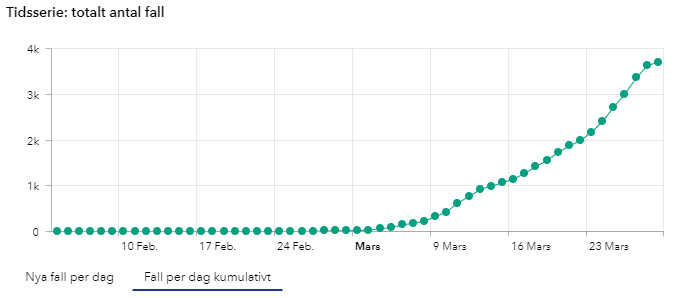
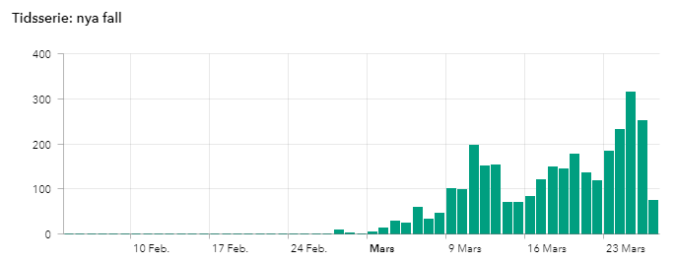
New confirmed cases daily in Sweden.
(Number of COVID-19 cases over time in Sweden, updates during mornings at 14:00 so todays numbers are not yet complete until the next day).

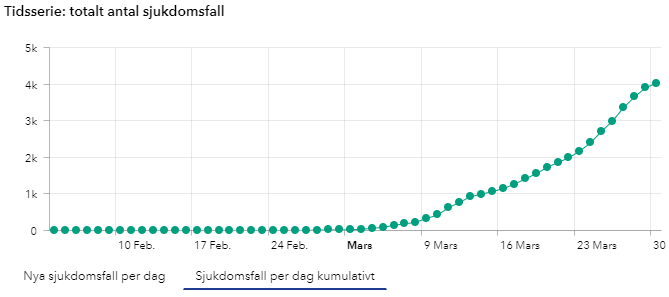
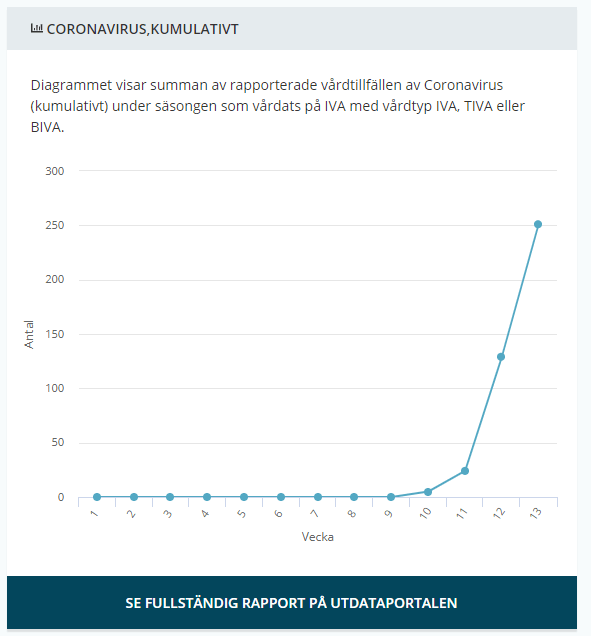
New confirmed cases accumulated over time in Sweden.
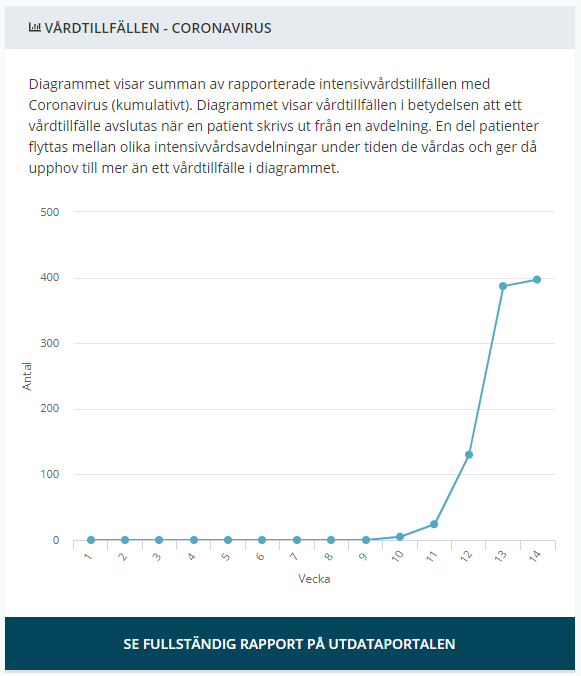
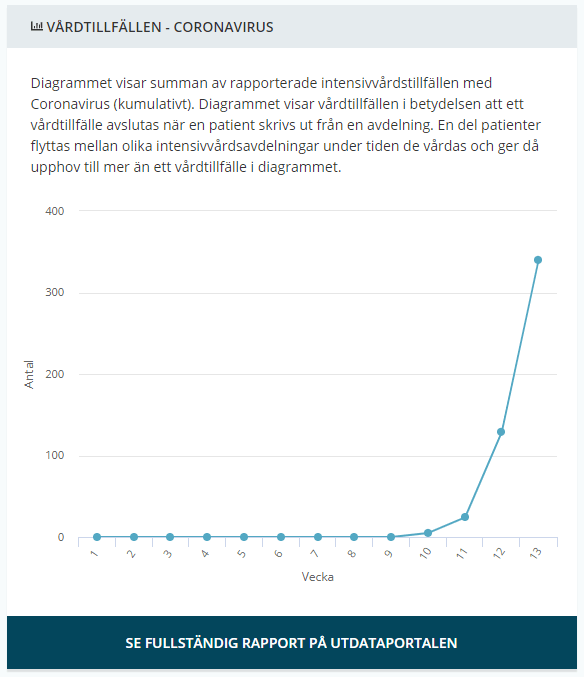
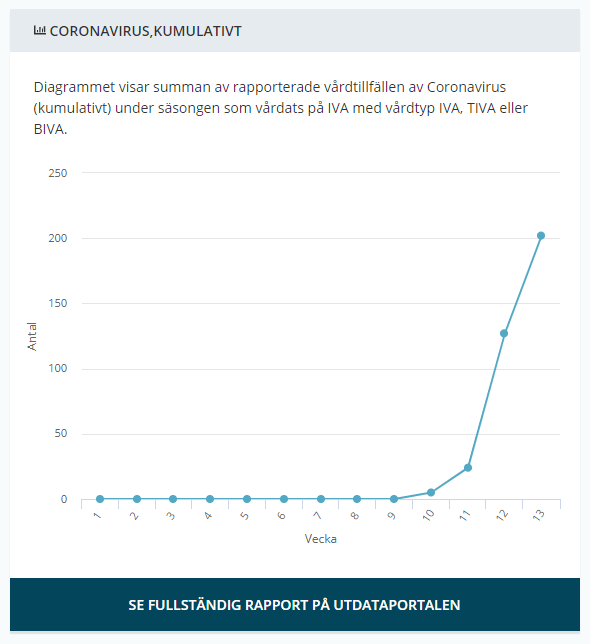
(Number of COVID-19 cases over time in Sweden, updates during mornings at 14:00 so todays numbers are not yet complete until the next day). - Intensive care Sweden: *
- 358 COVID-19 confirmed patients treated in the ICU in total so far
- 9,1 days from symptoms to ICU
- 24,9 % women

Total number of recorded of COVID-19 patients needing ICU care each week. From Week 10 it seems to more than triple each week, 5 → 24 → 130 → 413 → (464 this week up until now, however since it’s only tuesday this weeks numbers are yet incomplete)
COVID-19 Numbers Globally (updated today 2020-03-31 at 10:00 CET) *
- 33 673 confirmed deaths
- 719 758 confirmed cases
- 202 countries, areas or territories with cases
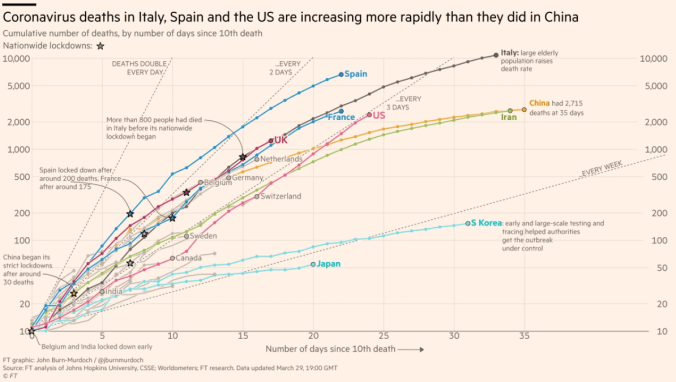
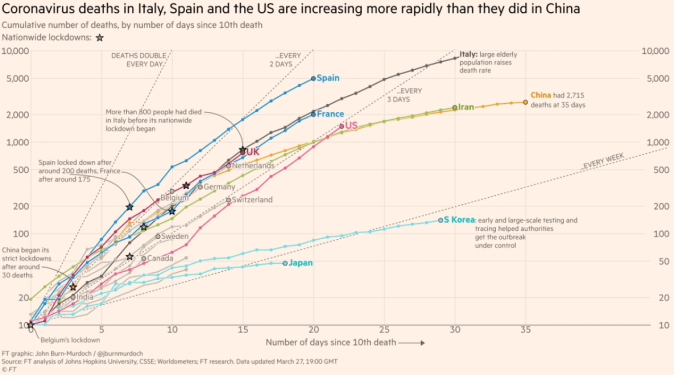
Financial Times Cumulative Number of Deaths Selected Countries (updated yesterday 2020-03-30 at 19:00 GMT) *

New Resources Added to ※ CTSOP
- Severe Outcomes Among Patients with Coronavirus Disease 2019 (COVID-19) — DAta from United States, February 12–March 16, 2020
Image [SWE]: Cheat Key for Patients With ARDS by Karolinska *
That’s it until tomorrow, keep calm and stay safe!